(serie de diapositivas utilizadas en clase)
Clasificacion De Las Enfermedades Cerebrovasculares
Isquémico
- Aterotrombótico
- Lacunar
- Embólico Cardiogénico
- Causa no precisada
- Otras
Hemorrágico
- Intraparenquimatoso
- Sub-Aracnoideo
Mas del 85% de los ACV hemorrágicos y 45% de los isquemicos están vinculados de algún modo con la hipertensión arterial.
- Serios daños en la pared arterial (arterioesclerosis), con dilataciones segmentarias especialmente en el territorio de la arteria silviana y muy especialmente en las tálamo-estriadas.
- Arterias tortuosas y se presentan placas duras y blandas, que a la vez se pueden complicar con obstrucciones o migraciones de elementos provenientes de su ulceración, generando embolias ha distancia.
â??La hipertensión arterial prepara y ejecuta la hemorragia cerebral â??
Las características clínicas más frecuentes del ACV, corresponden generalmente a la aparición súbita de cualquiera de los síntomas siguientes:
- Debilidad o torpeza en un lado del cuerpo
- Dificultad en la visión por uno o ambos ojos
- Severa cefalea no usual en el paciente
- Vértigo o inestabilidad
- Disartria y alteraciones del lenguaje
- Alteraciones de la sensibilidad
Conducta Médica en el ACV:
- Debe realizarse un examen neurológico rápido pero completo.
Este debe incluir: fondo de ojo y la flexión del cuello. - Las características clínicas del infarto (isquemia) pueden ser idénticas a las de la hemorragia: la hemorrágia puede asociarse más tempranamente a signos de hipertensión endocraneana; el infarto puede identificarse clínicamente un síndrome correspondiente a un territorio vascular específico.
Hipertensión intracraneana aguda
- Cefalea severa
- Depresión de la conciencia
- Nausea y vómito
- Diplopia horizontal
- Papiledema o hemorragias retinianas
- Irritación meníngea, Dolor y rigidez en cuello
- Fotofobia
- Ocasionalmente midriasis unilateral asociada incluso a un tercer par completo (ruptura de aneurisma de A. Comunicante posterior)
Realizar TAC de urgencia
Si aparece depresión de la conciencia antes de las 24 hs de ACV puede sospecharse:
- Hemorragia
- Hipoxia
- aumento de la presión intracraneana
- edema cerebral (infarto de gran tamaño)
- compromiso de tallo cerebral
- crisis epiléptica
ACV Hemorrágico
Factores de riesgo (no modificables)
- Edad
- Sexo
- Constitución
- Antecedentes familiares
- Raza
Factores de riesgo (modificables)
- Hipertensión Arterial (87%)
- Diabetes (especialmente la tratada en forma irregular y discontinua)
- Obesidad
- Dislipidemias
- Tabaquismo
- Stress
- Sedentarismo
Otros factores de riesgo
- Trastornos hemorrágicos y de la sangre: coagulación intravascular, diseminada, hemofilia, anemia drepanocítica, leucemia,niveles reducidos de plaquetas en la sangre.
- Consumo de aspirina o medicamentos anticoagulantes (diluyentes sanguíneos)
- Enfermedad hepática (que en general se relaciona con un aumento del riesgo de sangrado)
- Amiloide cerebral o tumores cerebrales
Factores Etiológicos
- Ateromatosis arterias tálamo-capsulares
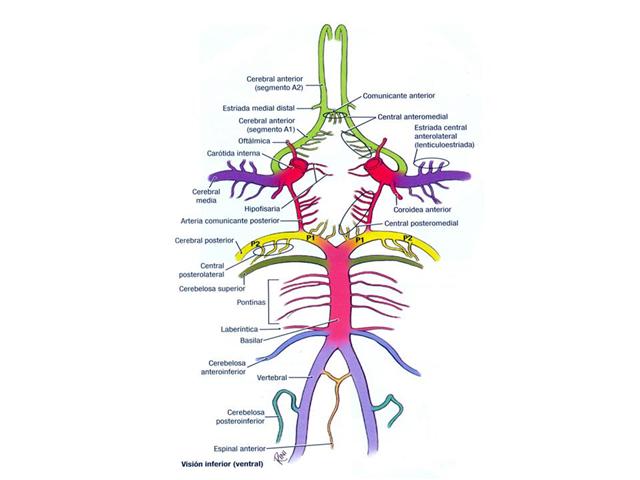
- Aneurismas arteriales del polígono de Willis
- Aneurismas arteriales micoticos (ramas secundarias)
- Malformaciones arterio-venosas
- Vasculitis
- Traumas
- Discrasias sanguíneas
- Tumores
- Anticoagulacion
- Uso de cocaína
Formas Clínicas
- Intra parenquimatosas
- Subaracnoideas
- Mixtas
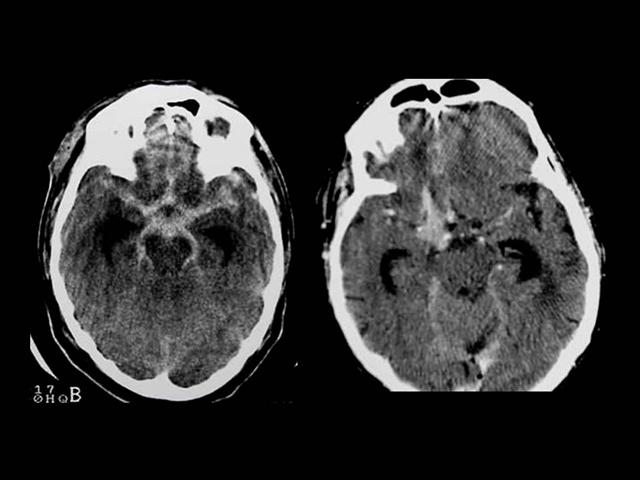
ACV Intra parenquimatoso
Afecta quinta y sexta década de la vida, evocan el clásico â?? derrame cerebralâ?, agudo, fulminante, sorprende al paciente en plena actividad o esfuerzo, con hemiplejía, alteraciones de la conciencia.
87% de los pacientes tienen antecedente de hipertensión arterial desconocida, no tratada o mal tratada.
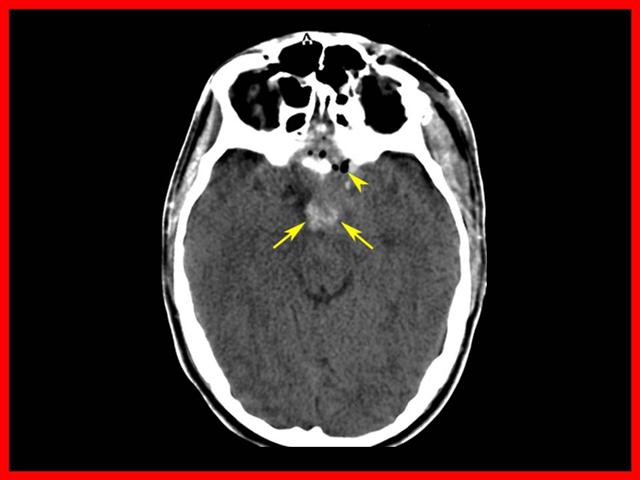
ACV Subaracnoideo
Es la variedad de adolescentes y adultos jóvenes, consiste en la irrupción aguda de la sangre en el espacio subaracnoideo, predomina en las rupturas de aneurismas del polígono de Willis.
Se inicia con una cefalea aguda de gran intensidad con síndrome meníngeo, vómitos centrales, fotofobia y raquialgia.
ACV Mixto
Es una combinación de las dos formas anteriores y son por lo general formas intra parenquimatosas volcadas al espacio subaracnoideo o malformaciones arteriovenosas.
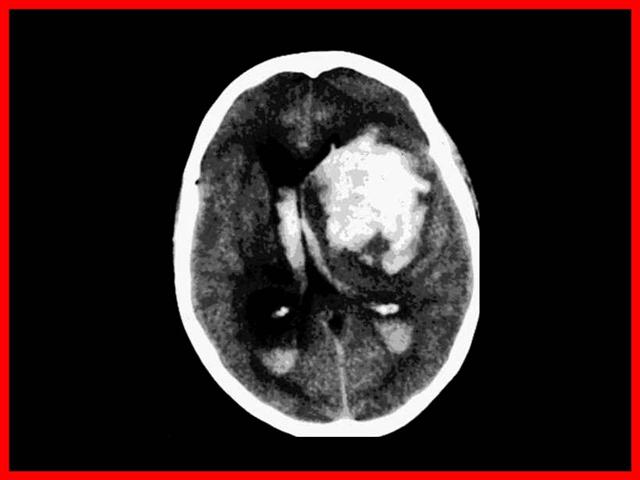
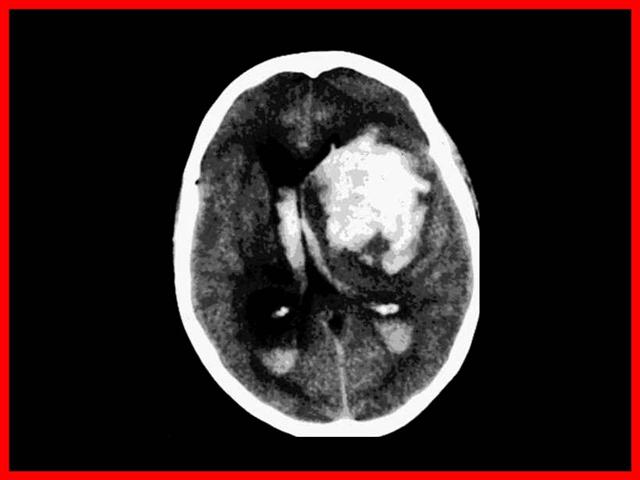
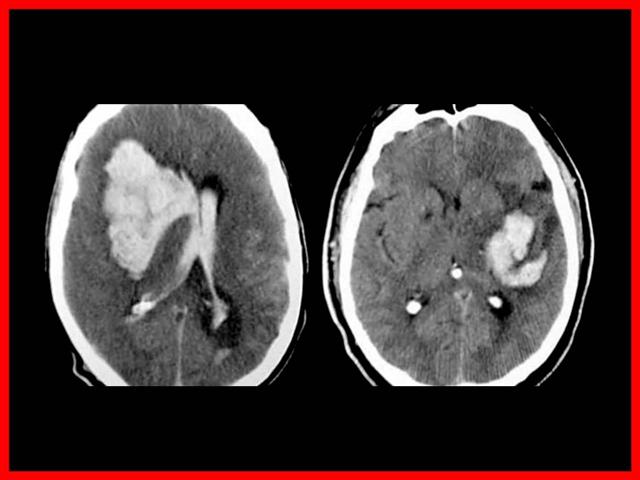
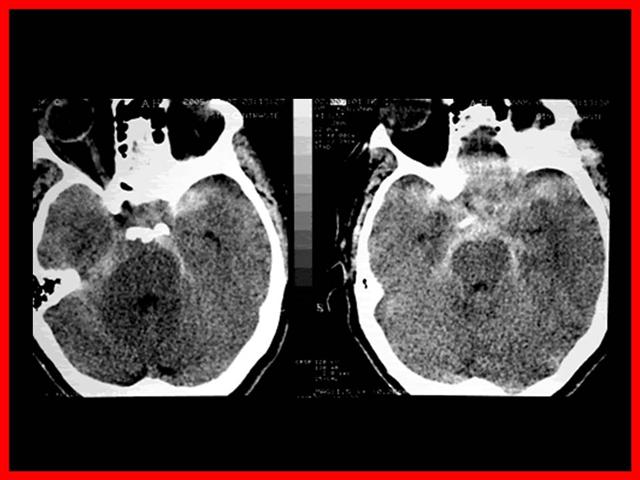
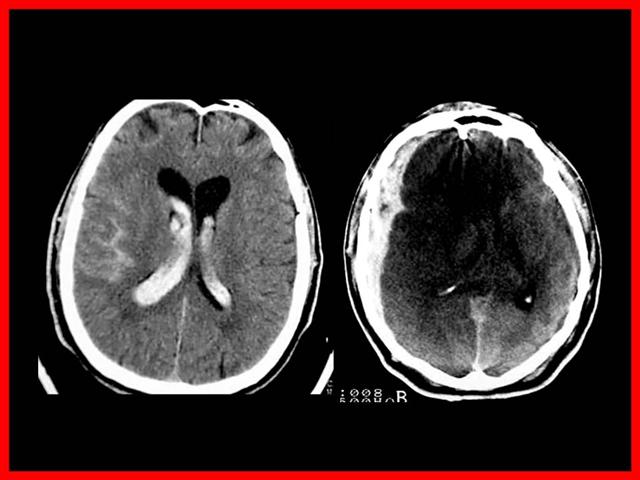
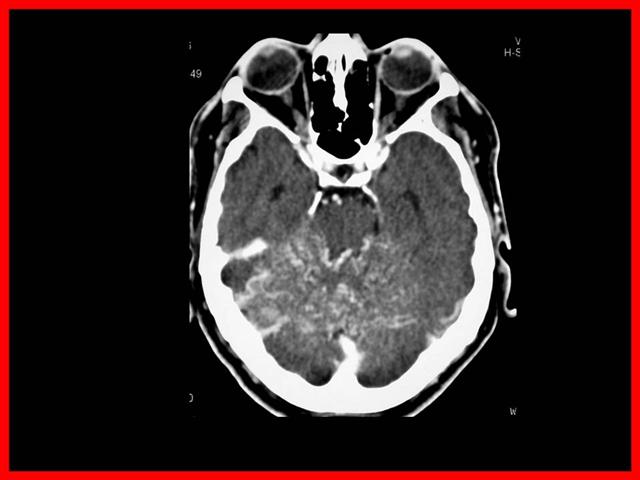
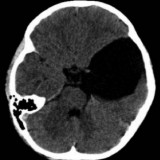
ACV Hemorrágico Intraparenquimatoso
Cuadro clínico
Cuadro fulminante, agudísimo (ictus) que sorprende al individuo en plena actividad, por lo general diurno, con severos trastornos de conciencia, hemiplejías facio braquio crurales, parálisis de la mirada conjugada â??mira hacia la lesiónâ?, etc.
Diagnóstico
- Quinta o sexta década de la vida
- Antecedentes de varios años de hipertensión arterial
- Diurno en plena actividad o esfuerzo
- Comienzo agudo, fulminante
- Frecuentemente cefalea inicial
- Hipertensión arterial al ingreso
- Alteración de conciencia
- Déficit motor evidente, hemiplejía facio braquio crural
- Ausencia de trauma o intoxicaciones
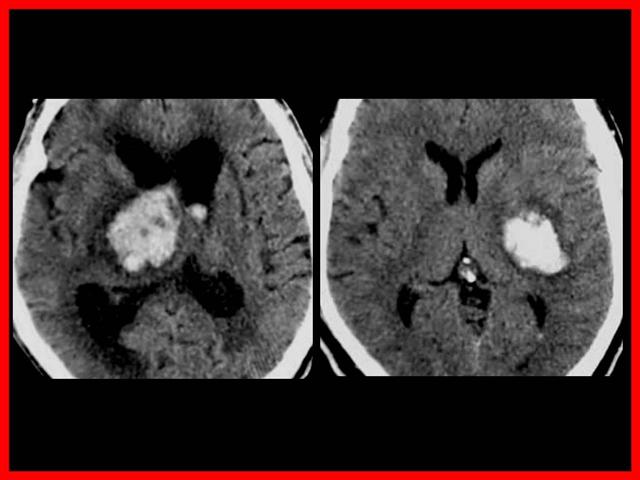
Topografía
- La mayoría de las hemorragias intra parenquimatosas se localizan en cápsula interna y núcleos basales (75%)
- Arterias penetrantes lesionadas por HTA: Putamen, Tálamo, Protuberancia, Cerebelo, Lobar (angiopatía amiloídea en ancianos).
Otras localizaciones son (25%):
- Frontales: predominan la confusión, excitación psicomotriz, alucinaciones, foco motor parcializado y atenuado (paresia) Apraxia motriz
- Parietales: hemiparesias con trastornos sensitivos Asomatognosia Alteraciones de conciencia de menor cuantía
- Occipitales: Hemianopsia homónima contralateral
- Temporal dominante: Afasia
- Tronco encefálico: Severas alteraciones de conciencia, trastornos respiratorios Hemiplejías alternas
- Cerebelo: Trastornos de conciencia, ataxia y dismetria ipsilaterales Síndrome de hipertensión endocraneana por Hidrocefalia obstructiva
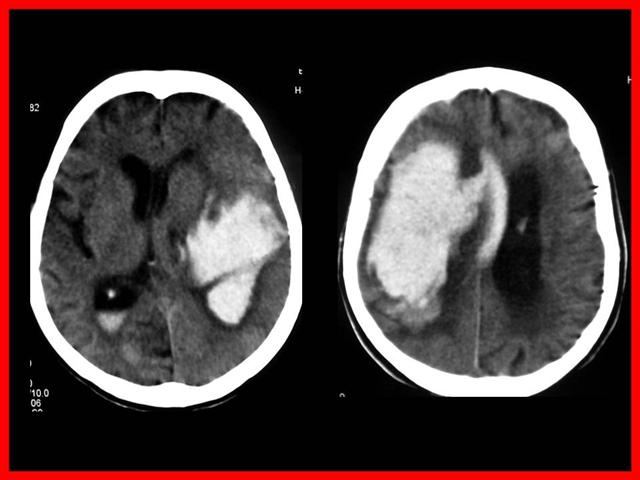
Si el TAC muestra hemorragia intracerebral:
- Determinar la causa posible
- Solicitar Panangiografía cerebral si se sospecha malformación arteriovenosa o tumor
- Solicitar valoración urgente por Neurología o Neurocirugía
- Solicitar valoración urgente por UCI si el Glasgow es de 8/15 o menor o si hay desviación de la línea media mayor de 5 mm o disminución de las cisternas perimesencefálicas
ACHh IP – Tratamiento Inicial
Los mejores resultados se obtienen cuando el paciente es manejado en forma multidisciplinaria y oportunamente, siendo fundamental que el aviso al especialista sea lo más precoz posible.
Los objetivos fundamentales son
- Salvar la vida
- Atenuar la magnitud del daño encefálico
- Evitar nuevas hemorragias
- Prevenir secuelas
- Asegurar las funciones básicas: reanimación, masaje cardiaco, respiración boca a boca, intubación aspiración de secreciones, etc.-
- Canalización pluriorificial
- Cabecera elevada a 30 grados
- Sintomático (analgesia, antitérmicos, sedación)
- Tratar la hipertensión arterial solo si supera los 220 mm de Hg.
- Evaluar derivación a centro de mayor complejidad. Sobre todo si hay compromiso de conciencia, progresión del daño neurológico, anisocoria, fracaso en el control de la hipertensión arterial o dificultades respiratorias
- Manitol al 15% ante la demora de evacuación a un centro especializado (100-150 cc a goteo libre)
Pronóstico
El pronostico en general es grave (Mortalidad de casi el 50% a las 48 hs.)
Se relaciona con:
- Ubicación de la lesión (pronostico peor para las profundas, para las del tronco y las volcados a ventrículos y/o que produzcan hidrocefalia)
- Tamaño de la misma
- Trastorno de conciencia grave (Mortalidad 90% ingreso en coma)â?
- Intensidad y duración de la crisis hipertensiva.
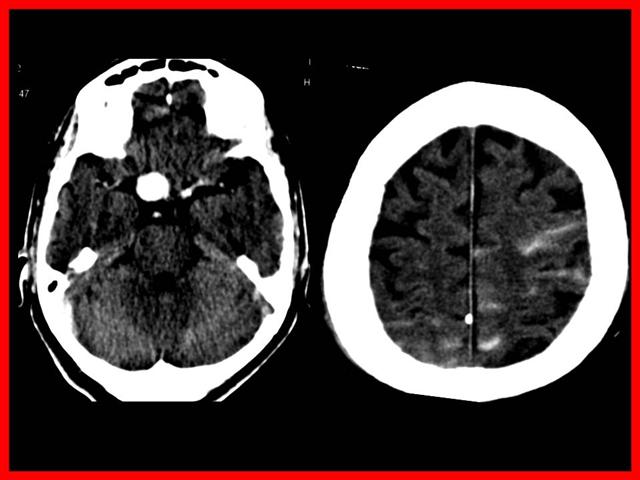
ACV Hemorrágico Subaracnoideo (HSA)
Diagnóstico
Lo más importante es pensar en su existencia
Estar muy atento a:
- Cefaleas moderadas a severas en personas jóvenes de comienzo brusco
- Cefaleas en las que se detecta un compromiso neurológico aunque sea mínimo
- No atribuir etiologías vagas, como de origen hepático o psíquico
- Síndromes meníngeos mínimos
Ante la duda internar al paciente, realizar tratamiento sintomático y sobre todo OBSERVAR la evolución, si persisten las dudas TAC standard y si no es posible punción lumbar
Si la detección es tardía o retrospectiva se debe aconsejar la consulta inmediata a un centro especializado con traslado en ambulancia con el paciente en reposo absoluto
Diagnóstico Diferencial
1- Con etiologías infecciosas causantes de síndrome meníngeo, especialmente meningitis purulentas:
- Iniciación más brusca
- Buen estado de salud previo
- Cefalea muy intensa
- Ausencia de síndrome general infeccioso
- TAC revela presencia de sangre en el espacio subaracnoideo
- Punción lumbar LCR hemorrágico
2- Con cuadros productores de déficit de conciencia con o sin signos focales neurológicos:
- HIP espontáneos: predominan signos de déficit neurológico y los trastornos graves de conciencia, pero no hay Síndrome meníngeo
- Procesos infecciosos, menningoencefalitis o abscesos: predomina lo séptico, no hay un comienzo hiperagudo y la cefalea no es brusca y de tan marcada intensidad, faltan los antecedentes vasculares
- TCE: es la causa más frecuentes de hemorragia subaracnoidea, hay signos de violencia y antecedentes traumáticos
3- Con cefaleas benignas tales como migrañas y cefaleas tensiónales
- Cronicidad y reiteración del cuadro cefaleico
- No hay rigidez de nuca y columna, a lo máximo reducción de la movilidad
- Por lo general conflictos y stress
- Frecuente contractura muscular de otras regiones
- No hay compromiso neurológico
HSA traumática con neumoencéfalo
Diagnóstico
- Tomografía Axial Computarizada
- Punción Lumbar
- Arteriografía de cerebral 4 vasos
Indicación de Punción Lumbar
- Cuadro clínico de Hemorragia Subaracnoidea sin posibilidades de realizar Tomografía Axial Computarizada.
- Cuadro clínico sugestivo de Hemorragia Subaracnoidea en presencia de signos no concluyentes en la Tomografía Axial Computarizada.
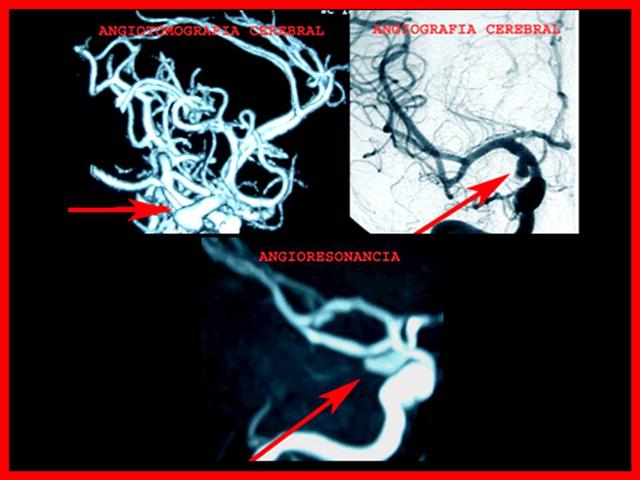
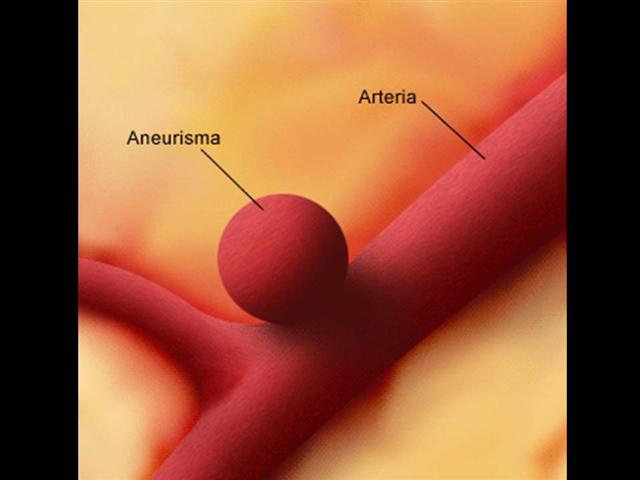
Aneurismas
Etiología y Epidemiología
- La principal causa de HSA es la rotura de un aneurisma intracraneano
- Los aneurismas arteriales congénitos son dilataciones debidas a ausencia congénita de la capa media y o remanentes embriologicos, que por lo general son pediculados y asientan en su mayoría en el polígono de Willis
- Se considera que entre el 1 al 2% de la población poseen esta malformación (autopsias); mientras que la incidencia de Hemorragia subaracnoidea por aneurismas es de 10-20 pacientes por 100.000 habitantes y por año
- Predomina en la cuarta y quinta década de la vida, con leve predominio del sexo femenino 3:2

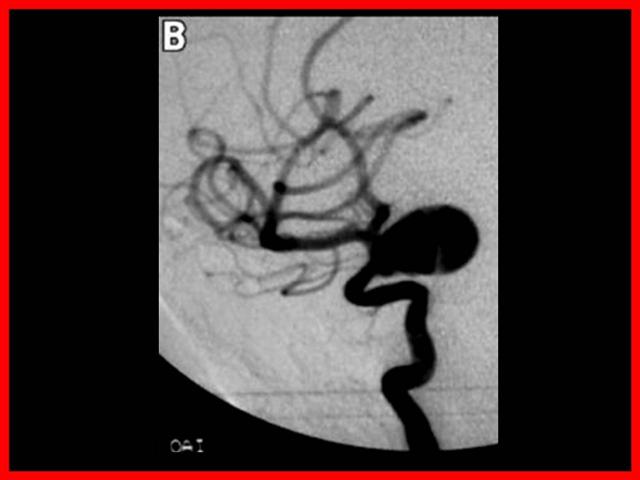
La localización ampliamente preponderante de los Aneurismas intracraneanos es en el polígono de Willis, situado en la base del cráneo y dentro de el:
- 33 % Complejo cerebral-comunicante anterior
- 33 % Sifón carotideo
- 33% Otras localizaciones
Entre 15-20 % tienen aneurismas múltiples
Clínica
- En algunas oportunidades y dado el crecimiento de estas malformaciones congénitas pueden dar síntomas neurológicos que resulten evocadores de su presencia
- Dado que la mayoría asientan en el polígono de Willis lo más frecuente son déficit de pares craneanos, especialmente el motor ocular común
- Otra situación son hallazgos incidentales con motivo de practicarse un estudio imagenologico por otra razón; estos pacientes deben ser referidos al especialista que evaluara el contexto anatómico, forma, tamaño, edad, estado general, etc. y recomendara una opción terapéutica personalizada
Conducta Médica
Si el TAC muestra hemorragia subaracnoidea:
- Escala Hunt y Hess
- Escala de Fisher
- Solicitar pruebas de coagulación
- Iniciar Nimodipina IV 3 cc/h y aumentar hasta 5-8 cc/h lentamente monitorizando TAM
- Iniciar fenitoína IV (125 mg c/8 hs)
- Solicitar Panangiografía cerebral
- Solicitar valoración urgente por Neurocirugía
- Solicitar valoración urgente por UCI si el Hunt y Hess es de dos o mayor o si el Fisher es de dos o mayor
Escala de Hunt y Hess
(tiene valor pronostico y guía el Tratamiento)â?
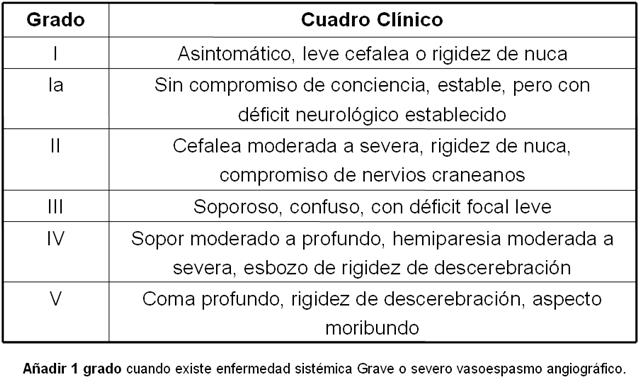
Escala de Hunt y Hess
Escala de Fisher
(Para evaluar vasoespasmo post – HSA)
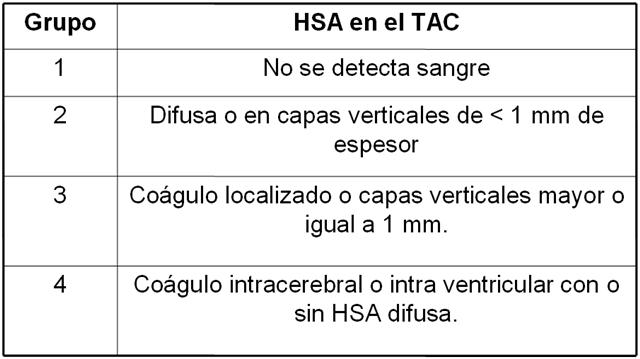
Escala de Fischer
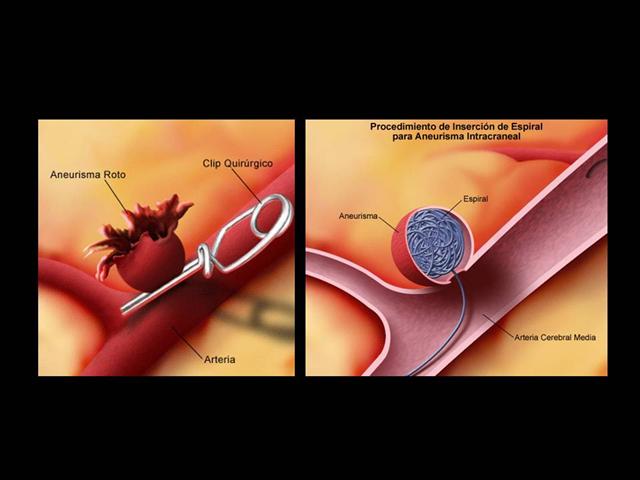
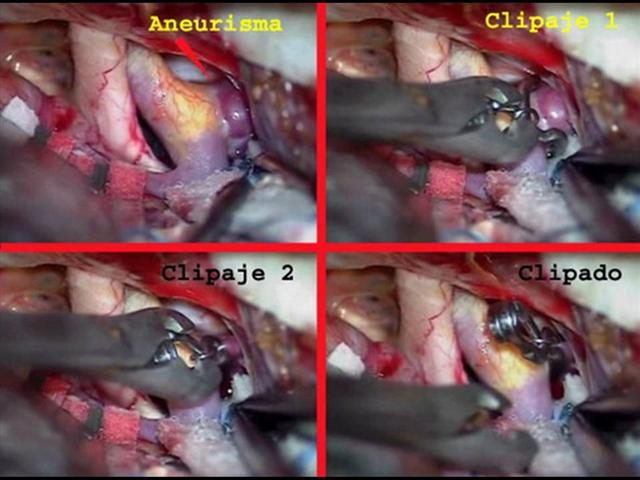
Tratamiento de los Aneurismas
- Clipado
- Embolización
Evolución
Complicaciones tempranas (0-3dias)
- Edema cerebral con desplazamientos
- Resangramientos
- Hidrocefalia aguda
- Disritmias cardiacas
- Disfunción respiratoria
- Edema pulmonar
Complicaciones mediatas (4-14 días)
- Vasoespasmo
- Resangramiento
- Hipovolemia
- Hiponatremia
- Hidrocefalia subaguda
- Neumonía
Complicaciones tardías (>15 días)
- Hidrocefalia crónica
- Neumonía
- Embolismo pulmonar
- Resangramiento
- Vasoespasmo cerebral
- Disbalance hidroelectrolítico
Factores asociados al resangrado
- Edad avanzada (> 70)
- Días 0-1 de la Hemorragia Subaracnoidea
- Pobre gradación neurológica
- HTA sistólica moderada o severa (170-240)
- Punción lumbar en presencia de Presión intracraneal aumentada
- Ventriculostomía para aliviar la PIC
- Asociada a hipertensión arterial sistémica
- Suspensión brusca de la terapia antifibrinolítica
- Intubación abrupta
Factores que predisponen la aparición de vasoespasmo
- Grandes hemorragias que llenan las cisternas basales
- Días 4-14 después de la Hemorragia Subaracnoidea
- Hiponatremia ( Síndrome cerebral de perdida de sal)
- Hipovolemia ( Disminución del volumen sanguíneo o de plasma)
- Hemorragia Subaracnoidea recurrente
- Agentes antifibrinolíticos
- Hipotensión arterial ( Disminución de volumen intravascular o inducida farmacológicamente)
- Presión intracraneal aumentada
- Otros ( Bajo gasto cardiaco, disrritmias, hipoxia, anemias).
Aproximadamente entre un 8-15% de los pacientes que sufren vasoespasmo fallecen durante las primeras 24 horas, sin recibir atención médica.
La mortalidad asciende a:
- 20-25% en las próximas 48 horas
- 44-56% en los 14 idas iniciales
- 66% de 1-2 meses después de la HSA
Pronóstico
Sin tratamiento
- Recidiva de la hemorragia; en general mas grave que la inicial, se estima entre el 3 y el 5% el riesgo anual
- ï? Déficit neurológico agregado por embolias generadas en el saco aneurismático que se impactan a distancia
- Oclusiones vasculares de vasos donde asienta el aneurisma
- Epilepsia parcial o focal
Con tratamiento
- Dependiente de la gravedad del cuadro inicial:
- Dependiente del trastorno de conciencia inicial
- Dependiente de la localización y tamaño
- Experiencia del centro especializado
- Experiencia de los neurocirujanos tratantes
- Experiencia en la elección del método terapéutico
Entre 15-30% no llega al Hospital
Coma profundo inicial: 87 % de mortalidad con o sin cirugía
Hallazgos incidentales con tratamiento en frio: 0,5% mortalidad y 2% morbilidad
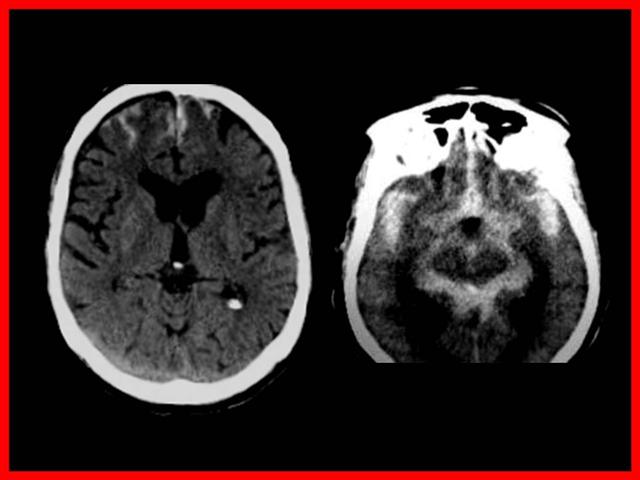
ACV Hemorrágico Mixto
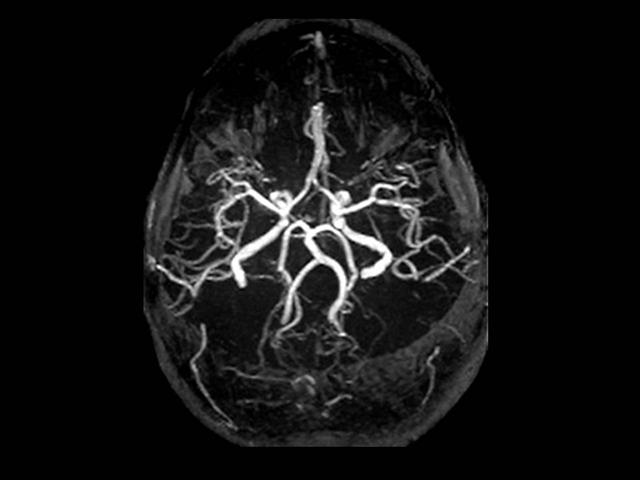
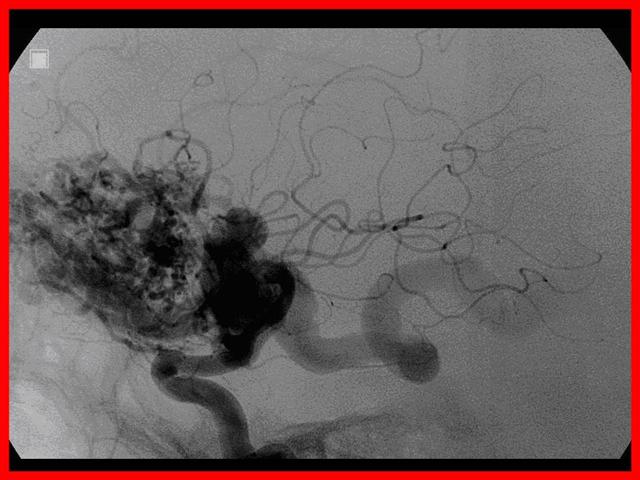
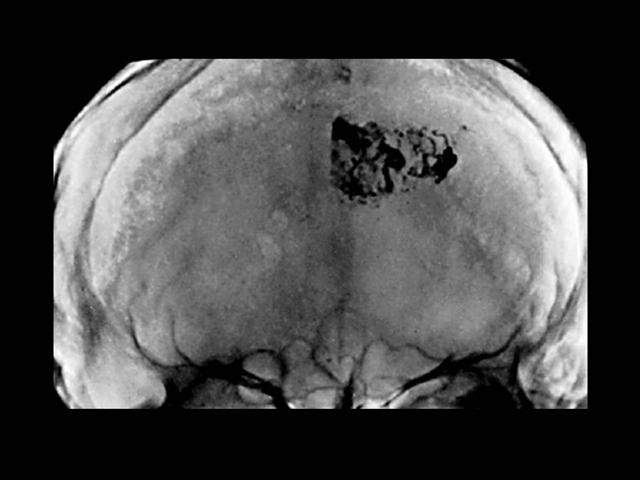
Malformaciones Arteriovenosas (MAV)
Agrupan a malformaciones de diversa índole:
- las verdaderas malformaciones arteriovenosas
- los cavernomas
- las malformaciones venosas
- las fístulas arteriovenosas durales
- y las telangiectasias capilares
Las malformaciones arteriovenosas están formadas por un ovillo de vasos dilatados que forman una comunicación anormal entre el sistema arterial y venoso, constituyendo una fístula areriovenosa.
Se trata de una anormalidad del desarrollo caracterizada por la persistencia de un patrón embrionario de vasos sanguíneos.
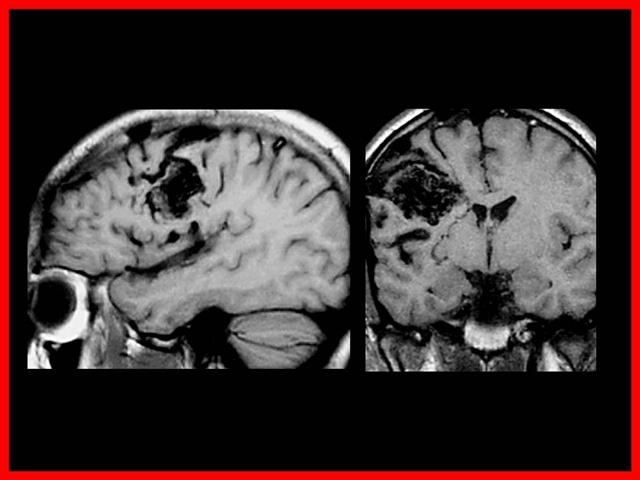
Clínica
La lesión está presente desde el nacimiento, el comienzo de los síntomas se produce habitualmente entre los 10 y 30 años.
La cefalea recurrente es una queja frecuente.
Pueden producir clínica neurológica a través de diversos mecanismos:
- En primer lugar la ruptura puede producirse en el espacio subaracnoideo, en los ventrículos cerebrales, pero se produce con mayor frecuencia en el parénquima cerebral.
- En ausencia de hemorragia, crisis epilépticas, un defecto neurológico progresivo se desarrolla como consecuencia de un fenómeno de robo del flujo sanguíneo o como consecuencia de un efecto de masa de la malformación.
- Se presentan en el 0,1% de la población, una prevalencia 10 veces menor que la de los aneurismas
- Son el 90% supratentoriales.
- El riesgo promedio de sangrado se ha evaluado en numerosos estudios de historia natural, estimándose en el 2-3% anual.
- Después de una segunda hemorragia el riesgo de resangrado puede aumentar hasta el 25%. Los datos clínicos y de neuroimagen en el momento del diagnóstico pueden ayudar a predecir el riesgo de sangrado futuro.
Las MAV pueden sangrar en:
- parénquima cerebral (60%)
- espacio subaracnoideo (30%)
- ventrículo (10%)
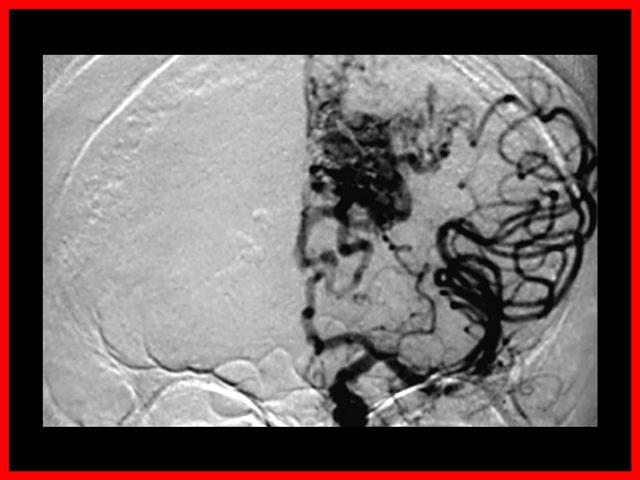
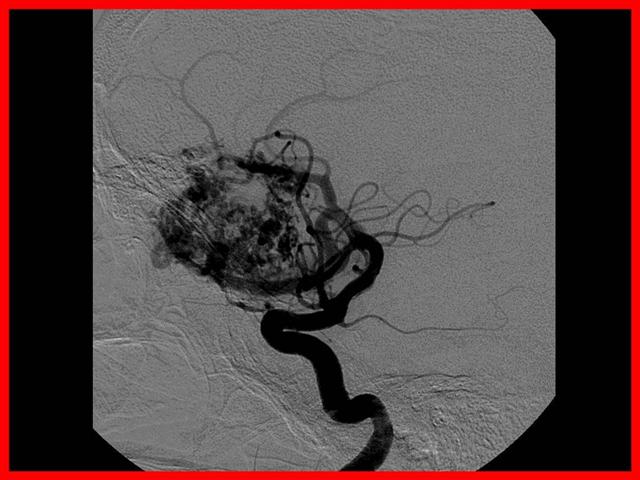
Diagnóstico
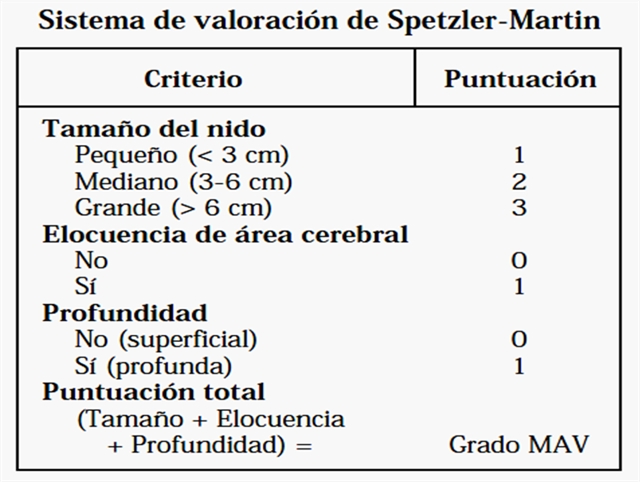
Clasificación de Spetzler - Martin
Tratamiento
- Depende de factores dependientes del riesgo vital del sujeto y de factores relacionados con la morfología, localización y tamaño de las malformaciones.
- La escala de Spetzler ayuda a valorar el riesgo de la cirugía.
- Según la valoración global se pueden utilizar los siguientes abordajes de forma aislada o en combinación.
Cirugía
Embolización
Radiocirugía
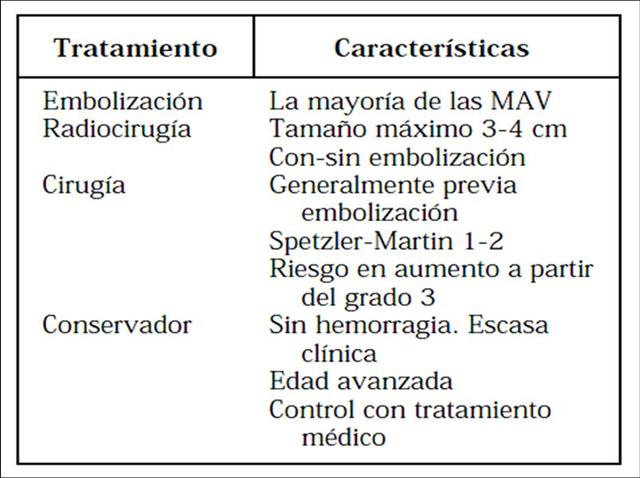
MAV - Embolización
Pronóstico
Sin tratamiento:
- Recidiva de la hemorragia (2-3% anual)
- Isquemias progresivas con aumento del déficit neurológico (fenómeno de robo)
- Hematomas intra parenquimatosos expansivos
- Hidrocefalia obstructiva (Aracnoiditis reaccional)
- Estado de mal convulsivo
Con tratamiento:
- Se evitan recidivas hemorrágicas
- Epilepsia: Crisis parciales, en gral. de fácil control
- Eventual aumento de déficit neurológico
Dr. Bernardo Sonzini Astudillo








me gustaria que me dieran informacion de neurofisiologia
DR. BUENOS DIAS HACE APROXIMADAMENTE 3 AÑOS ME OPERARON DE LA COLUMNA, PERO TENGO MUCHO DOLOR EN LAS CADERAS Y SIENTO COMO UNAS BOLAS O PELOTAS CUANDO ME TOCO, ME HACEN MASAJES Y ME AYUDA NUCHO PERO NUNCA DESAPARECEN, TAMBIEN TENGO MUCHOS CALAMBRES, NO SE SI ES POQUE TENGO PROBLEMAS CON LAS RODILLAS, PERO LO DE LA CADERA SI ME TIENE MUY MAL, QUE ME PUEDE AYUDAR, SALUDOS
ANTONIO SACHEZ
excelente esta pàgina.. mil gracias
permite un aprendizaje significativo
todo sobre los acv leannnnnnnnnnnnnnnnnf
acv todo¡¡¡¡¡¡¡¡¡¡¡¡¡